Lesson 9
Nutritional Needs

Compliance Indicator
The program provides for the nutritional needs of children in attendance at no additional cost to families. The meals are culturally and developmentally appropriate for the children being served and shall meet the nutritional requirements specified by the Child and Adult Care Food Program (CACFP) or the National School Lunch Program (NSLP).
Regulations/Reference
CCD Program Instrument: III. Program Quality CCD 13 Welfare & Institutions Code: 10208, 10210, 10240, 10250, 10251
Title 5: 18111 & 18278
Monitoring Review Evidence
Current Month Menu
List of Any Children with Food Allergies
Written Policies for Provision of Meals/Snacks
Watch Video Lesson ❯
Sample Forms/Tools ❯
Claims for Reimbursement
Infant Feeding Resources
Review Sketch Pad Notes ❯
Birth through 5 Months
For infants who are between the ages of birth through the end of 5 months, the only item that should be served is breastmilk or iron-fortified formula
Promote Breastfeeding

It is commonly known that breast feeding generally provides the best source of nutrients & helps protect infants against illnesses & chronic diseases.
For this reason, it is important to promote breastfeeding by providing a private & sanitary location that allows mothers to breastfeed their children or express milk to be stored such as:
Including a comfortable chair
Table
Access to running water & soap
Signage designating a private breastfeeding area
On-Site Breastfeeding

On-site breastfeeding must be documented. You may simply write on the menu or meal count form one of the following:
Infant was offered breastmilk
Breastfed on-site
Mother on-site
NOTE: No requirement to measure the amount of breastmilk a mother feeds her infant
Serving Milk

Types of Milk
Parent may choose to provide expressed breast milk for caretaker to serve to their infant while in care
ORIf a child is not being fed breast milk, iron-fortified formula is the best alternative
Serving Milk
Feed on demand
Avoid force-feeding
Serve a minimum of 4-6 fluid ounces at each meal (Note that some infants may not consume the entire serving)
6 Months through 11 Months
For infants who are between the ages of 6 months through 11 months, meal planning requires more consideration, as this is the time that solid foods are introduced into the infant’s diet.
Ready for Solid Foods?

While there is no exact way to determine when an infant is developmentally ready to accept solid foods, there are a few guidelines that may be helpful:
Sits in seat with good head control
Opens mouth when food comes their way
Moves food from a spoon into their throat
Doubled their birth weight
NOTE: Most infants are capable of these skills at approximately 6 months, but it may be as late as 7 or 8 months.
Introducing Solid Foods

Once an infant is ready to accept solid foods AND you have communicated with the parent(s), offer food to the infant using the following guidelines:
Gradually introduce solid foods, one at a time & over the course of a few days or weeks
Ensure food has appropriate texture & consistency
Always watch for allergic reactions
NOTE: It is not necessary to offer an infant a solid food component at every meal until the infant has established a tolerance for that food component.
Meal Patterns
Meal pattern requirements for infants ages 6 months through 11 months are as follows:
Breakfast, Lunch & Dinner

For breakfast, lunch & dinner, all components must be offered:
Breast Milk or Formula
Fruit/Veggie
Grains
Meat/Meat Alternative
Snack

For snack, 3 components must be offered:
Breast Milk or Formula
Fruit/Veggie
Grains
Special Rules/Limitations
To ensure nutritious meals are being served, there are rules or limitations that apply to the type of beverage or food item being served within the meal components.
Formula

If a child is not being fed breast milk, iron-fortified formula is the best alternative.
There are two main requirements to remember when supplying formula to infants in your care.
Offer at least one variety of iron-fortified formula
It must be a formula that is regulated by the FDA
Fruits & Veggies

Fruits & vegetables are an essential source of nutrients such as fiber & various vitamins.
Caretakers are required to incorporate 0 to 2 tablespoons of fruits, vegetables, or both into all meals & snacks.
Meats & Meat Alternates

Low-fat meat & meat alternatives such as yogurt, whole eggs, cheese & dry beans are also an important component of infant meals because they provide protein.
Eggs
Whole egg must be served
Serving size is 0 to 4 tablespoons
Yogurt
0 to 4 ounces or a ½ cup is considered one serving
May only be served once daily
Pay attention to serving sizes & “sugars” or “added sugars”
NOT more than 23 grams of sugar per 6 ounce serving
Cheese
0 to 2 ounces of cheese is considered one serving
Many varieties available
No “cheese foods” or “cheese products”
Grains

Within the grain component, cereals may served to children as part of a meal or snack; however in order to be considered reimbursable, cereals must not contain more than 6 grams of sugar per dry ounce
NOTE: An easy way to determine if the cereal is acceptable is to use WIC approved cereals
Modifications
Sometimes infants have disabilities, allergies, or conditions that prevent them from being able to consume a particular food item, such as iron-fortified formula.
Medical Statements
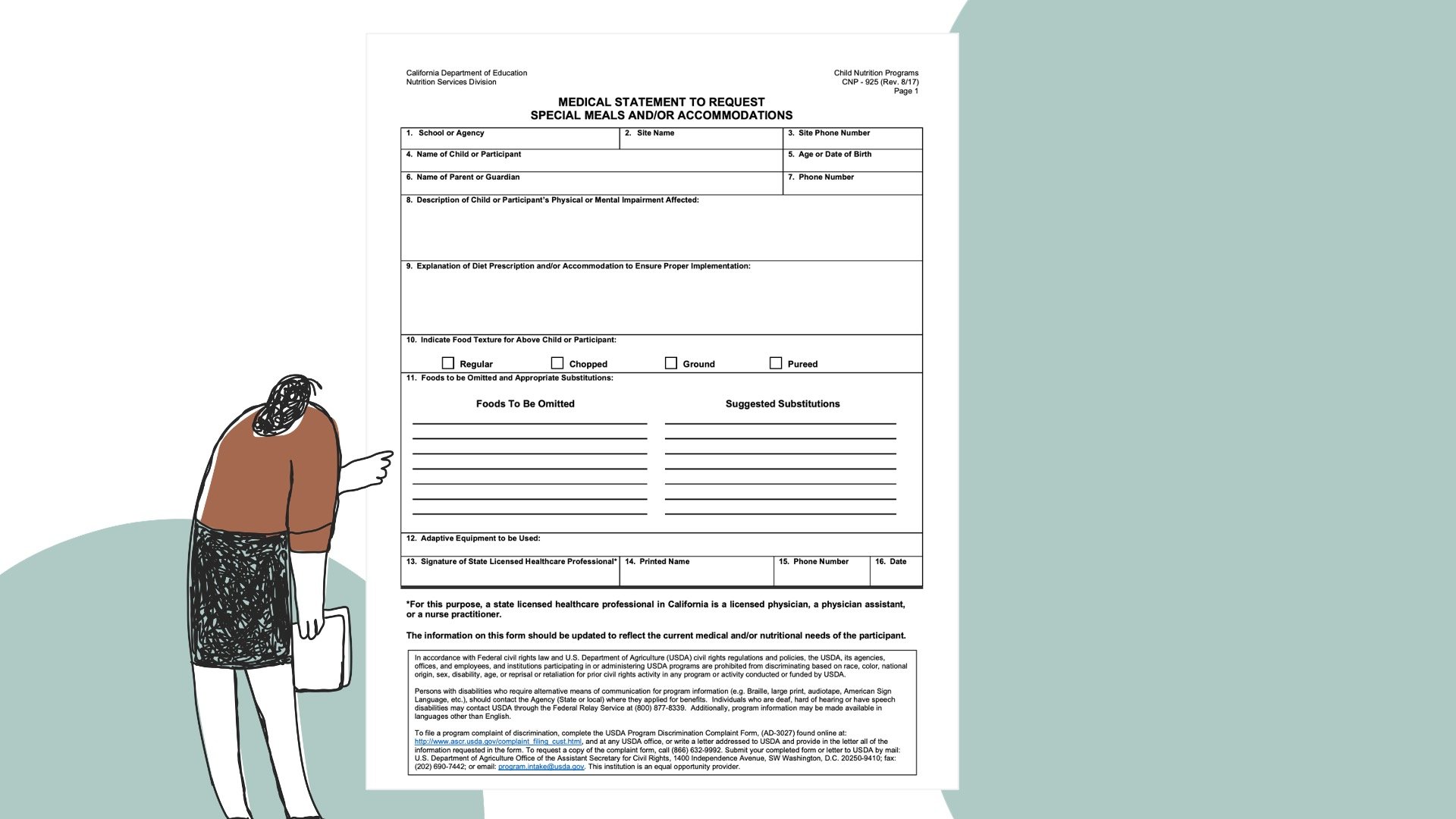
Medical Statement is only required when modifications do not meet the meal pattern requirements
Medical Statement is required when a meal modification calls for serving a specific food or an entire meal that does not meet the meal pattern requirements
A medical statement should include two key features:
Information describing child’s disability & how it affects their diet
Alternative formula or food
Review Medical Statements carefully & keep on file
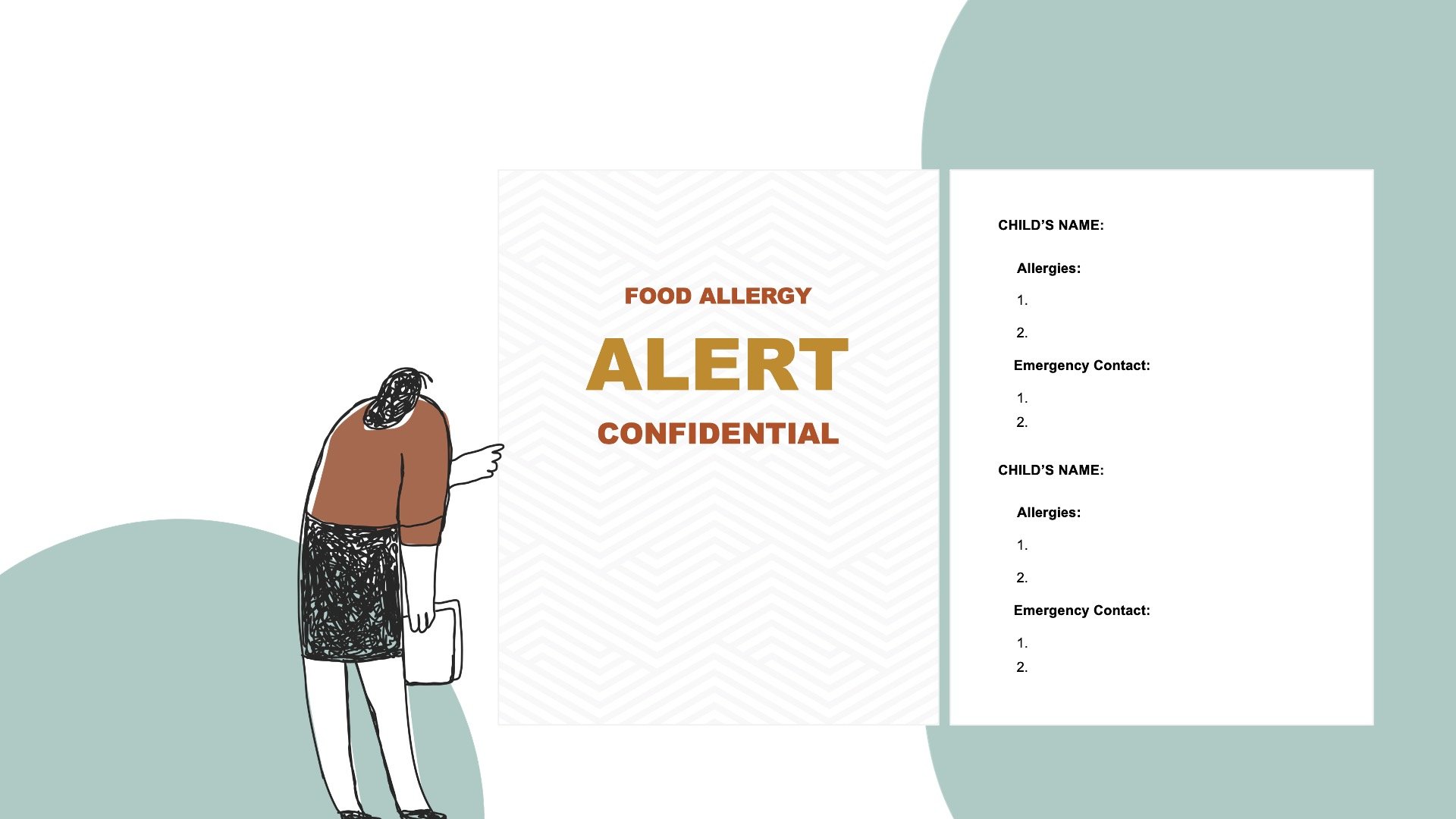
Ensure the posted food allergy alert is current & staff are very familiar with children who have milk or food allergies
Other Resources

Access many CACFP trainings & resources available on the Institute of Child Nutrition’s website located at theicn.org

Claims for reimbursement are submitted on CNIPS, the web-based system for administering nutrition programs
Complete Knowledge Check ❯
After reviewing the video lesson & sketch pad notes, it’s time to check for understanding by completing a Knowledge Check. Note that Individual Knowledge Checks will conclude with a Certificate.


